
Fundamentally, a vaccine functions similarly to an immune system cheat sheet. Vaccines provide your body with a sneak peek of the enemy without the full negative effects of bacterial or viral infection. Before you ever come into contact with the disease, your immune system learns to identify and combat it.
How does this immunological conditioning take place, then? We will answer this question in the blog, as well as the different classifications of vaccines. In the end, you will know more about how vaccines protect you and why it is crucial to create different vaccines for various illnesses.
But first;
What Are Vaccines?
A vaccine is an innovation in medicine developed to jumpstart your body’s immune system into action. It aims to defend you against a specific ailment but does not give you the ailment. Like other immunomodulators, it maintains and increases the capacity of the body’s immune system to fight off infections such as bacteria or viruses.
So how does this happen? First, a comparatively harmless variety of pathogens are introduced into the body. This teaches the body how to identify and attack the pathogen before it can attack.
And how are vaccines made? By using a living bacteria or viruses or a fragment of the pathogenic organism, such as its protein.
Vaccines are among the most significant achievements in public health. They play an important role in halting the epidemic of infectious diseases and many others.
Now, there are different types of vaccinations that can be administered depending on the nature of the disease, the individuals that need to be protected, and the level of protection that your body would require at any one time. Of course, each method has its strengths and weaknesses which we will be discussing shortly.
Why Vaccines Work
Your body’s own defense mechanism is your immune system. It consists of an intricate web of tissues, organs, and cells that cooperate to protect you from dangerous intruders such as bacteria, viruses, and other diseases.
Your immune system attacks when a pathogen enters your body because it perceives it as an alien body. However, this leaves your body at risk of getting infected. So, instead of sitting like a duck and waiting to be attacked, vaccines teach your body how a pathogen would look and how to defend itself against potential infection. This way, your immune system is always on high guard.
And in order to teach your immune system to identify and eliminate a pathogen without causing illness, vaccines expose you to a weakened form of the pathogen or a portion of it.
This is made possible by the fact that your immune system can “remember” a pathogen after it comes into contact with it, allowing your body to swiftly combat and eradicate it before it causes illness. When a real pathogen attacks, the immune system is already familiar and attacks right away.
So to comprehend more why vaccines work, let’s look at the classifications of vaccines below.
6 Classification of Vaccines and How They Work
There are several types of vaccines, and each one trains the immune system to combat illnesses in a unique way. Every vaccination type—from conventional live-attenuated vaccines to state-of-the-art mRNA vaccines—has a different strategy for priming your body for an actual infection.

Knowing these six classifications of vaccines makes it easier to understand the science underlying disease prevention and why doctors use various types of vaccines for various medical conditions.
Now, let’s examine each type of vaccine, how it operates, and the factors that contribute to its efficacy.
1. Live-Attenuated Vaccines
In live-attenuated vaccinations, a weakened or “attenuated” strain of the disease-causing virus or bacteria is used. This means that although the bacteria or virus is still alive, it has been modified in a lab to weaken it and prevent it from seriously harming a healthy body. It’s like putting your immune system through basic training.
Example of this vaccinations therefore include:
- The vaccine for measles, mumps, and rubella (MMR)
- The vaccine for varicella (chickenpox)
- Vaccine against yellow fever
- OPV, or oral polio vaccination
Thanks to live-attenuated vaccinations, measles and chickenpox outbreaks have been successfully avoided.
How They Work
When you take a live-attenuated vaccine, the weakened pathogen enters your body and begins to reproduce. Although it is in a weakened state and does not cause illness, it is still potent enough for your immune system to detect it.
Your immune system will identify the infection, make antibodies, and develop memory cells. Your body prepares to fight off the next time it comes into contact with the actual, full-strength virus or bacteria.
Advantages
- Robust and long-lasting immunity: Live-attenuated immunizations often produce lifetime protection after just one or two treatments. The immunological reaction resembles that of an infection that occurs naturally.
- You wont need frequent boosters with this vaccine for it’s robust immune response.
Cons
- Not suitable for all. Those with compromised immune systems, such as those receiving chemotherapy or living with HIV, may experience complications with live-attenuated vaccines. Even a weakened virus could be harmful to these people.
- Requirements for storage: These vaccinations usually need to be kept cold, which might make transportation and storage more challenging in some regions of the world.
2. Inactivated Vaccines
Inactivated vaccinations use viruses or bacteria that have been totally destroyed or rendered inactive, as opposed to live-attenuated vaccines. There is no possibility that these bacteria can cause the disease because they are unable to reproduce in your body. Even though the immune system isn’t working, it can still recognize the pathogen’s appearance.
Inactivated vaccinations are, for example:
- Vaccine against inactivated polio (IPV)
- The vaccination for hepatitis A
- Vaccine against rabies
- Influenza (flu vaccination)
How They Work
Heat, chemicals, or radiation destroy the germs in inactivated vaccinations. But, the immune system can still identify the pathogen’s external proteins or carbohydrates and launch an immune response even after it has died.
And compared to live-attenuated vaccinations, the immune response is weaker and less durable since the pathogen cannot multiply. In order to sustain protection, inactivated vaccines may call for several doses or booster shots over time.
Advantages:
- Safety: Vaccinated people, including those with compromised immune systems, are not at risk of contracting the disease because the virus or bacteria is dead.
- Extended shelf life: Inactivated vaccines are easier to store and transport since they are more stable than live-attenuated vaccinations and don’t need refrigeration.
Cons:
- Weaker immune response: Compared to live-attenuated vaccines, inactivated vaccines do not elicit as robust or durable protection. In order to stay protected, booster shots are frequently required.
- Additional dosages are needed: Typically, several doses of an inactivated vaccination are required to attain complete immunity.
When safety is a primary concern, such as for individuals with weakened immune systems or for illnesses where a dead pathogen is as efficient in boosting immunity, doctors prefer inactivated vaccines.
3. Subunit, Recombinant, Polysaccharide, and Conjugate Vaccines
Instead of exposing your immune system to the entire disease, these vaccines are more like a snapshot of it. Only fragments of the pathogen, such as a protein or sugar from its outer surface, are used in subunit, recombinant, polysaccharide, and conjugate vaccines to elicit an immune response. They are quite safe because they don’t include live components.
These vaccinations include:
- Subunit of the hepatitis B vaccination
- Recombinant human papillomavirus (HPV) vaccination
- Polysaccharide and conjugate pneumococcal vaccination; conjugate meningococcal vaccine
How They Work
These vaccines infuse the body with isolated antigens—the portions of the pathogen that cause an immune response—instead of the entire virus or bacteria. For instance, only one protein from the outer coat of the virus is present in the hepatitis B vaccination. Your immune system produces antibodies against this protein because it perceives it as an alien invader. Your body will recognize the protein and know how to combat the hepatitis B virus if you ever get exposed to it.
Subunit vaccinations employ particular fragments of the bacteria or virus. Through genetic engineering, recombinant vaccines are created by generating the necessary antigens from innocuous bacteria or viruses.
The sugar molecules present on the surface of bacteria are used by polysaccharide vaccines to boost immunity. Conjugate vaccinations strengthen young children’s immune responses by attaching polysaccharides in a carrier protein.
Advantages:
- Extremely safe: These vaccinations are unlikely to result in negative responses or side effects because they only use particular elements of the pathogen. Additionally, those with compromised immune systems can safely use them.
- Effective in the populations it is intended for: Since infants and young children don’t often react well to polysaccharide vaccines, conjugate vaccines are particularly effective at building high immunity in these populations.
Cons:
- Subunit and combination vaccines may need booster shots to maintain long-term immunity because they may not provide the entire pathogen.
- Difficult to produce: Compared to conventional procedures, the production of these vaccines can be more costly and complex.
Due to their safety profile, doctors prefer to use subunit, recombinant, and conjugate vaccines for protecting young children, the elderly, and people with weakened immune systems.
4. Toxoid Vaccines
Some illnesses are brought on by the toxins that the infection produces rather than the pathogen itself. Instead of attacking the bacteria or viruses that cause these toxins, toxoid vaccinations are made to neutralize them.
Examples of toxoid vaccines are:
- The tetanus vaccine
- Vaccine against diphtheria
How They Operate
Inactivated toxins, known as toxoids that have been altered to render them incapable of causing harm are present in toxoid vaccinations. Your immune system still creates antibodies against the toxoid because it perceives it as a danger. Your body will be prepared to neutralize the poison before it can do any harm if you are ever exposed to the actual one.
Advantages
- Effective against toxin-based diseases: These vaccinations are very successful in avoiding illnesses like diphtheria and tetanus that are brought on by bacterial toxins.
- Secure and steady: The negative effects of toxoid vaccinations are few, and they are safe.
Cons
- Requires frequent boosts: Booster doses are frequently needed for toxoid immunizations in order to sustain immunity. The tetanus vaccine, for instance, should be administered every ten years.
- Restricted use: These vaccinations only work against illnesses brought on by toxins, not the infections themselves.
Toxoid vaccines show remarkable efficacy for illnesses, especially when the symptoms are brought on by other toxins rather than a direct bacterial or viral infection.
5. mRNA Vaccines
Although mRNA vaccines have been under research for a long time, the COVID-19 pandemic brought them to the world’s attention. mRNA vaccines generate a protein linked to the pathogen rather than a virus. And in response to that protein, your immune system becomes ready to combat the virus itself if you come into contact with it.
mRNA vaccines include:
- BioNTech-Pfizer COVID-19 vaccine
- The COVID-19 vaccination of today
How They Work
Messenger RNA, a genetic fragment found in mRNA vaccines, contains instructions for your cells to produce a protein. Often, they spike protein present on the virus’s surface. Your immune system then launches a defense by creating antibodies and memory cells after your cells make this protein, identifying it as alien. Eventually, no portion of the virus remains in your cells since your body breaks down the mRNA itself after it has completed its function.
Advantages:
- Quick development: mRNA vaccines may be created and manufactured in a short amount of time, which was very helpful during the COVID-19 epidemic.
- No live virus is necessary: The vaccination is extremely safe because no live virus is used, thus, there is no chance of contracting the illness.
Cons
- Distribution may become more difficult due to the need for ultra-cold storage conditions for mRNA vaccines.
- New technology: Although the technology underlying mRNA vaccines has been researched for years, their general application is still relatively new, and long-term data is still being gathered.
mRNA vaccines is a major advancement in vaccine technology providing a versatile and effective means of combating newly emerging illnesses.
6. Viral Vector Vaccines
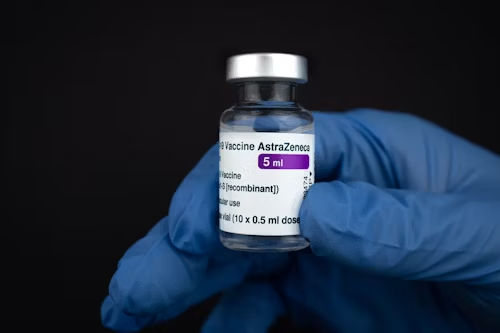
Viral vector vaccines transfer a portion of the pathogen’s genetic material into your body by means of a harmless virus, typically a modified adenovirus. This benign virus, also known as a vector, instructs your cells to make a pathogen-associated protein, which in turn sets off an immunological reaction.
Viral vector vaccines are, for instance:
- AstraZeneca Oxford The COVID-19 vaccination
- The COVID-19 vaccination from Johnson & Johnson
How They Work
A modified virus that is incapable of replicating or infecting people is used in the viral vector vaccination. This virus introduces genetic material from the pathogen into your cells, including the SARS-CoV-2 virus’s spike protein. Once within, the protein is produced by your cells as directed. After identifying this protein as alien, your immune system launches an attack.
Advantages:
- Robust immunological reaction: Viral vector vaccines, like live-attenuated vaccines, elicit a strong immune response by simulating an actual infection.
- Beneficial during pandemics: Viral vector vaccines are a useful tool during emerging disease outbreaks because they may be generated fast.
Cons
- Pre-existing immunity: The vaccination may be less effective in certain individuals who already have immunity to the viral vector (such as adenoviruses).
- New technology: Long-term data is still being collected for viral vector vaccines, which are also very new, similar to mRNA vaccines.
Because viral vector vaccines can elicit robust immune responses, they present a viable strategy for quickly generating vaccines against novel illnesses.
Conclusion
It’s evident from our exploration of the different classification of vaccines that not all vaccines function in the same manner. Every vaccine type ranging from live-attenuated and inactivated vaccinations to innovative mRNA and viral vector vaccines has advantages and disadvantages.
While certain vaccines are better suited for those with weakened immune systems, others are best for providing long-lasting immunity. While some can be dispersed more readily in isolated locations, others need to be kept in extremely frigid temperatures.
And if we know how vaccinations operate and the motivations behind their creation, we can better appreciate the complex science that keeps us safe and healthy.
The various classifications of vaccines will continue to be at the vanguard of our defense as we confront new threats to world health, whether they come from newly discovered viruses or illnesses that we have fought for millennia.
Remember, vaccines are not merely a relic from the past; they are an active, developing aspect of contemporary medicine that will keep saving lives for years to come.
Get Cutting-Edge Bioreactors from Bailun Technologies!
Are You Prepared to Increase your Vaccine Production?
Modern bioreactors made for accuracy, scalability, and efficiency are available from Bailun Technologies if you want to improve your capacity to produce vaccines. Our bioreactors offer the dependable, regulated conditions required to grow cells and viruses at scale, whether you’re creating conventional vaccinations or developing the newest advancements in mRNA or viral vector technology.
Select the best for your vaccine manufacturing, and don’t skimp on quality. To find out more about our cutting-edge vaccine bioreactor solutions and how they help speed up your manufacturing process, get in touch with Bailun Technologies right now.
Together, let’s make life-saving vaccines a reality! You may feel secure knowing that decades of research, development, and a thorough comprehension of the immune system’s amazing capacity to maintain your health are behind that tiny syringe the next time you roll up your sleeve for an injection.

